Dear Friends,
With Passover almost upon us, we trust that following the recent 20th-Knesset elections, the country will unite for the benefit its citizens. We also hope that the Israeli health system will get the targeted attention it deserves to address our highest priority patient care needs.
Supporting our staff so they can support our patients
In our ongoing drive to recruit and retain the most skilled patient care professionals, we are planning to construct a residential tower for our dedicated staff members. The tower will hopefully resolve housing availability and affordability issues that our staff faces, with a solution in close proximity to the Medical Center. It will also help make essential clinical staff members, nurses and physicians available quickly during critical events, such as mass disasters that require immediate response.
The tower, which will have 19 floors plus parking, will cost over $40 million to construct. Apartment rental will cost about 20-25% less than average rental costs in the hospital neighborhood. A donation of about $5 million will help launch construction; the Medical Center will fund most of the remaining costs with a long-term loan to be repaid with apartment rental fees.
Financial giving that endures
Recently, we were fortunate to receive several most generous bequests from friends who lived full lives and donated funds and resources in their wills for the benefit of Medical Center patient care. We value their thoughtfulness and humbly honor their selfless acts. Read more about these bequests below.
As you read about our outstanding clinical and scientific initiatives, we wish you and your families a happy Passover and a joyful spring!
Yours in friendship,
Ronit Blum
CEO, Association of Friends, Tel Aviv Sourasky Medical Center
Terror attack in Tel Aviv a sober reminder of trauma preparedness
A recent stabbing attack in Tel Aviv recounts the unsettling events of a decade ago, when the Medical Center was on the front line for treating victims of terror attacks that were rampant in the city.
In late January of this year, a terrorist boarded a bus on a busy downtown street and stabbed 19 riders, including the driver, before being subdued. The wounded were treated at Tel Aviv Sourasky Medical Center, with three in serious condition. Fortunately, the rest were only moderately or lightly injured. All victims have since been released from the hospital.

Every incident like this is a reminder that Tel Aviv Sourasky Medical Center must be trained and ready for any eventuality in order to provide immediate life-saving trauma care.
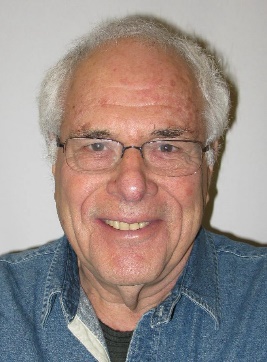
In memory of Avraham Pressler, the advocate for Holocaust survivor hospitalization conditions
Avraham Pressler, the revered representative of the Conference on Jewish Material Claims against Germany, passed away in November 2014 at the age of 90. Until his final days, Pressler worked tirelessly for the benefit of Holocaust survivors.

Image: From right to left: Avraham Pressler, Prof. Gabi Barbash, and Rabbi Julius Berman at the appreciation ceremony for Pressler a short time before his passing.
In 2000, Pressler invited Dr. Rabbi Israel Miller, of blessed memory, then President of the Claims Conference, for his first tour of the Ichilov Hospital Founder’s Building.The tour highlighted for Dr. Miller the dire need to improve the physical conditions in the internal medicine departments, where a high percentage of Holocaust survivors were being treated.
The transition to state-of-the-art facilities
Since Miller’s visit, in an effort that has taken about 15 years, the Claims Conference has helped build 5 new internal medicine departments, 2 geriatric rehabilitation departments, the General Intensive Care Unit, and the Neurosurgery Department, and helped procure equipment for the Ambulatory Emergency Wing and Physiotherapy Institute. These upgrades have helped the Medical Center’s facilities remain in step with the outstanding patient care provided at the facility.
We will remember Avraham Pressler’s distinct image, his faithful activities for Holocaust survivors and his partnership in upgrading patient hospitalization conditions at Tel Aviv Sourasky Medical Center. May his memory be a blessing!
Donations
Charitable bequests: leaving a legacy
Recently, the Tel Aviv Sourasky Medical Center was honored to receive donations for important initiatives from generous people who bequeathed contributions in their wills. Most of these committed donors were friends of Tel Aviv Sourasky Medical Center for many years. We were saddened by their passing, and appreciate their thoughtfulness for choosing to bequeath financial resources to the Medical Center:
- Moshe Boroshek: Approximately $1.7 million
- Rina Aharoni: Approximately $4 million
- Natan Steer Adler: Approximately $2.3 million
- Baruch Shechter: Bequeathed his apartment, which was sold for $615,000
- Tzipora Kasten: Bequeathed approximately $1 million
May their memory be a blessing.
What’s new?
OrbiShape: a revolutionary internal bra to support long-term breast-procedure results
Breast procedures are growing in popularity and demand. However, existing surgical techniques pose challenges in quality and result duration. Available techniques rely on the skin to support the weight of the breast after surgery. But as gravity takes its course, breasts lose their fullness and re-sag.
Plastic surgeons often face declined patient satisfaction after several months of follow up. Moreover, experts estimate that more than 40% of women consider breast surgery, but many are reluctant to undergo the procedure due to concerns of non-lasting results and potential scarring.
Enter OrbiShape: a breast-support implant
Developed by Professor Eyal Gur, OrbiShape is a novel breast implant designed to resolve the inherent problems in current reconstructive plastic surgery procedures, such as breast reduction, breast lift and breast symmetrization.
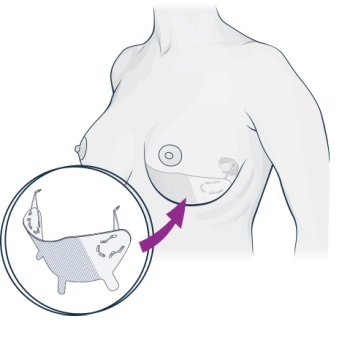
OrbiShape is a medical-grade silicone sling that is easily and painlessly inserted and anchored to the ribs during the final step of the breast procedure. It is the only proven solution available for anchoring soft breast tissue to bone. OrbiShape is aiming to become the new standard of excellence in plastic and reconstructive breast surgeries.
Because the sling serves as an “internal bra,”
it has key benefits, such as long lasting results and better breast projection. And since OrbiShape supports breast weight and eliminates the pressure on the suture line,
it potentially minimizes scar visibility.
Proven success
After over 100 OrbiShape procedures performed and six years of satisfied patient follow-ups, leading surgeons in Europe are embracing OrbiShape. They are establishing a community of experts, training others and promoting the device around the world.
OrbiShape received the European regulatory compliance CE mark in 2013 and will undergo Food and Drug Administration (FDA) review for use in the U.S. next year.
About the developer
Prof. Eyal Gur is Head of the Reconstructive and Aesthetic Surgery Department at Tel Aviv Sourasky Medical Center. Professor Gur was selected by Newsweek magazine several years ago as one of the top 10 micro-surgeons in the world. He is Professor of Surgery in the Sackler Faculty of Medicine at Tel Aviv University and has authored over 70 papers and articles.
Microbiota: researching the importance of microorganisms to the human body
In recent years, the medical community has dramatically improved its understanding of the importance of microbiota to human health. Microbiota research is revolutionizing medicine, offering new therapies and insights on the factors that drive human health and disease.
Elucidating the role of gut microbiota in drug-induced liver injury (DILI)
A project by Prof. Oren Shibolet, Director of the Liver Unit in the Gastroenterology Department, funded by the Grass Foundation, is investigating the role of microbiota in drug toxicity in the liver. Drugs known to cause liver damage were given to mice raised without gut bacteria (germ-free). The study found significant changes in drug metabolism and liver toxicity between the germ-free mice and control mice harboring normal gut bacteria. The project will detail mechanisms responsible for the effect of microbiota on drug metabolism and will devise ways to manipulate microbiota to pave the way for individual patient-tailored medical treatment.
Fecal microbial transplantations effectively treat enteric bacterial infections
Fecal microbial transplantation is approved for treating C. difficile infections, which are the most common cause of hospital-acquired diarrhea. C. difficile is a major cause of morbidity and mortality within the elderly hospitalized patient population due to widespread antibiotic use. Antibiotics disrupt the normal gut flora, allowing C. difficile to colonize in the intestinal tract. Up to 10% of C. difficile patients do not respond to multiple antibiotic regimens and many of them die.
A high success rate

Recent research has shown that a simple fecal microbial transplantation (FMT) procedure eradicates C. difficile in up to 90% of the cases, proving more effective than standard antibiotic treatment. The newly established Bacteriotherapy Service, under the direction of Dr. Nitsan Maharshak, performs FMTs through a colonoscopy or gastroscopy. The service maintains a bank of frozen stool preparations donated by meticulously screened donors for patient procedures and research. The stool bank enables safe and immediate treatment without the need to find and screen donors. The protocol is approved by the Israeli Ministry of Health and the service has successfully treated 7 C. difficile patients.
Future applications
Prof. Zamir Halpern, Head of the Tel Aviv Sourasky Medical Center Digestive Disease Center comments, “FMTs have tremendous potential for treating other diseases, such as inflammatory bowel diseases (Crohn's disease and ulcerative colitis), obesity, diabetes, irritable bowel syndrome and more.” The Bacteriotherapy Service is soliciting grants and donations to cover the costs of performing further research.
The flicker frequency device helps test for minimal hepatic encephalopathy
Cirrhosis, the end-stage of all liver disease, occurs when liver tissue is replaced by scar tissue, causing multiple complications. Hepatic encephalopathy (HE) is a serious debilitating neuro-cognitive disorder caused by cirrhosis in which patients become disoriented and confused, have personality changes and can even become comatose. Encephalopathy occurs because the failing liver cannot clear blood toxins, which reach the brain and affect its function.
Early-stage hepatic encephalopathy
Minimal hepatic encephalopathy (MHE) is a very early stage of HE in which patients with cirrhosis seem and behave normally. However, sophisticated tests can uncover subtle cognitive dysfunction. MHE severely affects cirrhotic patient quality of life and day-to-day functional capacity. It has a significant influence on the patient's ability to drive.
The paucity of symptoms and lack of patient understanding of the situation make this condition very hard to diagnose. Thus, MHE patients may continue to drive, endangering themselves and others. MHE treatment includes medication and dietary interventions aimed at reducing blood toxin levels.
Improving patient functioning through testing, diagnosis and treatment

Prof. Oren Shibolet, Director of the Liver Unit in the Gastroenterology Department, describes the state-of-the-art diagnostic methods for MHE: “Current tools for MHE diagnosis use computer-based inhibition tests and the innovative ‘flicker’ device, which measures subtle changes in the patient's ability to identify flickering light. In this test, the patient wears special goggles which transmit either steady or flickering light. The patient is asked to report when the flickering light appears. Patients with MHE have great difficulty in identifying flickering light.”
The Liver Unit recently acquired the HEPAtonorm™ Analyzer device for flicker testing. Dr Helena Katchman is launching Israel’s first clinical service to diagnose and treat MHE. Treatment will help improve the patient functioning, quality of life and ability to drive safely, reducing the risk of traffic accidents for these patients.
Pain Clinic receives legal settlement funding
A legal settlement was reached in the Medical Center’s lawsuit against Merck Sharp & Dohme for Vioxx, the painkiller that had severe unreported cardiovascular side effects. Merck Sharp & Dohme has committed to donate about $3.7 million to renovate the Chronic and Acute Pain Center, under the leadership of Dr. Silviu Brill.
A round of applause
Prof. Zelig Eshhar, Chairman of Immunology at the Medical Center, to be awarded the Israel Prize ("Prass Yisrael") in Life Science Research
On Israel’s Independence Day, the Ministry of Education will award the Medical Center’s Prof. Eshhar the Israel Prize in Life Science Research for his discovery and development of a groundbreaking method to treat disease, specifically cancer. His recent human immune system discoveries have led to cancer treatments and are the basis for the development of new generations of biological medications for cancer and other diseases.
Prof Eshhar’s lab serves as the seed for the Medical Center’s Center of Cancer Research and Therapy, in collaboration with the Department of Bone Marrow Transplantation and Hemato-Oncology Department H. Prof. Eshhar’s accomplishments have been featured in previous Medipost publications.
Prof. Zelig Eshhar earns the Teva Award for Excellence
The Teva Award for Excellence, jointly given to Prof. Yehudit Bergman, was awarded in November 2014 in memory of Eli Hurvitz, former Teva CEO, for groundbreaking research in immunology.
Dr. Ido Wolf, Director of Medical Oncology Research, awarded Teva grant

Congratulations to Dr. Wolf, who won the Teva Research Grant: Groundbreaking Discovery Award in Biology that Contributes Directly to Medication Development – for developing a new mechanism for acquired resistance using hormonal treatment for breast cancer. The Teva prize is awarded annually based on recommendations from the Israel Science Foundation to researchers who excel—specifically for their commitment and collaboration with Israeli science and research.
Research excellence
Mastering hospital antibiotic resistance and its spread into the community
Dr. Yehuda Carmeli, the Head of the Department of Epidemiology and Preventive Medicine and a world-renowned expert in antibiotic resistance, is the principal investigator and/or co-investigator on several large, multinational research projects in defeating hospital antibiotic resistance and its dispersion into the community.
One such project is the EU initiative, DRIVE-AB, launched to encourage new antibiotic development to treat antibiotic-resistant bacteria (against which old drugs are no longer effective) and to develop new economic models to promote antibiotic development and encourage responsible use. Medical Center researchers are creating mathematical models to predict the spread of antibiotic resistance in 5, 10 and 20 years to help drug developers identify targets for new antibiotics.
Paving the way for novel for breast cancer therapy: from bench to bedside
Estrogen receptors are expressed in about 75% of breast cancers, and are the target for several of the most effective anti-breast cancer therapies. However, virtually all metastatic breast cancer patients who initially respond to hormone treatments eventually develop treatment resistance.
New estrogen receptor mutation more resistant to endocrine treatments
Tamar Rubinek, Manager of the Tel Aviv Sourasky Medical Center Oncology Laboratory, participated on a research team that identified a new mutation in an estrogen receptor in patients who developed endocrine resistance. They found that this mutation, D538G, was only present in metastatic tumor samples obtained from the liver, not the breast. The high prevalence of the mutation, which makes the receptor more active and resistant to endocrine treatments, may be relevant to patients who develop resistance.
Finding effective methods against cancers that harbor the mutation
Chemotherapy is currently the only treatment available for patients with endocrine-resistant breast cancer, but it is highly toxic and less effective that endocrine therapies. Preliminary findings suggest that inhibiting major breast-cancer-promoting molecular pathways may be effective against breast cancers harboring the D538G mutation. The next step is to study a large cohort of patients during different disease stages to determine the best therapeutic strategy to inhibit breast cancer cells that have acquired the mutation. This study was published in the journal Cancer Research.
Brain tumors potently activate the immune system: new findings provide a glimpse of hope
The brain has a special relationship with the immune system, the body’s natural defense against invaders. The strength with which the immune system reacts to immune challenges within the brain is usually less than that in the rest of the body. Joint research by Tel Aviv Sourasky Medical Center and Weizmann Institute researchers has led to an innovative approach whereby injecting brain tumor cells in locations outside the brain stimulates an immune system attack strong enough to affect even the brain. In animals, such an attack prolonged animal survival and even induced complete brain tumor regression.
Given the potential of this work for human brain cancer treatment, the organization ABC2 is funding a new clinical trial that will be conducted at Tel Aviv Sourasky Medical Center to test this type of therapy in humans – termed split immunity. In a small, safety-focused trial, patients with glioblastoma will receive injections of irradiated and intact live tumor cells from their own brain tumors and will then be monitored for immune activation and an anti-tumor response. If this approach is successful, it could pave the way for future clinical studies to further enhance treatment efficacy.
Grass Foundation supports liver research
In August 2014, the Grass Foundation generously awarded Prof. Oren Shibolet, Director of the Liver Unit in the Gastroenterology Department and Dr. Ido Nachmany, Director of the Surgery Department, one million dollars for liver research. The grant is being applied to advance the following basic science and clinical research in Hepatology and Hepatobiliary-pancreatic (HPB) surgery.
The role of CCAAT/enhancer-binding homologous protein (CHOP) in a liver cancer model: hepatology project by Prof. Shibolet
Liver cancer is the fifth most common cancer and the third cause of cancer-related deaths worldwide. A recent study assessed the role of CHOP, a key protein affecting cell survival, in regulating tumor growth. In a liver tumor model, mice lacking this crucial protein had smaller liver tumors compared to regular mice. The team is currently investigating the specific mechanisms by which CHOP mediates its action. Preliminary results suggest that the mTOR pathway, an important cellular cascade, is activated. The findings point to an important drug target, which may lead to better treatments for this deadly tumor.
Hepatobiliary-pancreatic surgery: research by Dr. Ido Nachmany
The Division of General Surgery is the largest and most advanced surgical service in Israel, leading the country in a broad range of surgical procedures and serving as a national HPB surgery referral center. The department’s exceptionally large patient volume and variety provide a unique opportunity for studying various aspects of tumor development and progression.
The Grass Foundation award will seed the state-of-the-art basic research laboratory to study molecular processes in HPB cancers. The lab will focus on hepatobiliary tumors, with special interest in both primary and secondary liver cancer.
Patient research will utilize "next-generation sequencing" combined with computational analysis to genetically characterize pancreatic, biliary, and primary and secondary liver cancers according to clinical treatment response and course of disease. DNA from both tumor samples and circulating peripheral-blood will be sequenced and compared with healthy tissue DNA. Integrating this genetic data with patients’ clinical courses and treatment responses will enable the research team to pinpoint key genetic features associated with disease progression and outcome. These features will then be evaluated in tumor patients to determine the best surgical and non-surgical therapy options. Providing the opportunity for patient-specific tailored therapy, these findings could revolutionize surgical oncology patient treatment.
Genome-wide characterization of the escape from tumor dormancy: spotlight on immature myeloid cells: research by Dr. Ido Nachmany and Dr. Niv Pencovich
Research has shown the dormant tumors exist in otherwise healthy individuals. These tumors can be present as one of the earliest stages in cancer development, during the tumor metastasis stage, and with residual disease following primary tumor treatment.
In order to progress and metastasize, tumors require the formation of proper blood vessels. The vascularization process that enables a dormant lesion to transform into a vascular outgrowing malignant tumor is commonly referred to as the "angiogenic switch.” Immature myeloid cells (IMCs) have played key roles in the angiogenic switch, tumor progression and spread. The team recently demonstrated that unique gene expressions dictate the recruitment of IMCs into malignant versus dormant tumors. In addition, preliminary research results in mice suggests that specific gene expression signatures in IMCs found in the peripheral blood may reflect specific stages in tumor progression and can be used as biomarkers for tumor growth.
The team’s goal is to shed light on the molecular mechanisms by which tumor cells interact with IMCs. Various molecular aspects of these interactions will be evaluated, aiming to pinpoint specific therapeutic targets and potential biomarkers for tumor progression.
New services
New radiosurgery facial pain-relief treatment for trigeminal neuralgia
Trigeminal neuralgia is one of the most severe neurologic pain disorder, characterized by sudden attacks of severe facial pain, which severely affects quality of life. The pain is usually unilateral, affecting the cheeks, jaw, teeth, gums, lips and occasionally around the eye or forehead. Pain episodes may appear spontaneously, but are usually triggered by a light touch around the mouth or face or by talking, eating or brushing one's teeth.
A nerve compression problem
Doctors believe that trigeminal neuralgia is caused when an artery from the brainstem compresses the trigeminal nerve, the nerve that supplies sensation to the face. The classic neurosurgical procedure for patients who don’t respond to medical treatment is microvascular decompression (MVD) surgery, which moves the nerve away from the offending blood vessel. This open brain surgery procedure has a high success rate, but also carries risk and is not appropriate for elderly patients or patients with severe comorbidities.
Effective least-invasive treatment
Stereotactic radiosurgery (SRS) is a well-established, minimally invasive trigeminal neuralgia treatment. It delivers precise, highly accurate, controlled radiation beams near the trigeminal nerve’s exit from the brainstem. This treatment, which damages the trigeminal nerve to stop the transmission of pain signals, is an ambulatory procedure that does not require anesthesia. About 80% of patients have initial reduced pain; about 50-60% of the patients have sustainable long-term pain relief.
Collaborative procedure using state-of-the-art equipment
The collaboration between the Department of Neurosurgery and the Institute of Radiotherapy enables treatment for patients from all over Israel on 4 newly-acquired leading-edge linear accelerators.
Ending unnecessary needle sticks: the new laser technology that locates kids’ veins easily

In its continuous commitment to patient care and quality of life, especially for kids, the Dana-Dwek Children’s Hospital has recently implemented a device to minimize needle sticks. The innovative AccuVein400 (AV400) device helps the medical team locate patient veins and target the exact needle insertion location for drawing blood or inserting an intravenous line.
A simple laser projector
The handheld infrared laser device reveals veins under the skin and projects a laser image on the skin’s surface. The medical team uses the laser “drawing” to pinpoint the right size vein and location. 
According to Dr. Ronit Lubetzky, the Director of the Children’s Department at Dana-Dwek, “Patient blood draws, especially when we’re talking about children, present a significant challenge in locating veins, and often requires several attempts. Now, with the AV400, the care team can more easily locate the veins to minimize needle sticks, which reduces kids’ fear of needles and anxiety related to the staff.”
Introducing the Multidisciplinary Center for Congenital Bone Diseases and Bone Health in Children and Adolescents
The first of its kind in Israel, the Multidisciplinary Center for Congenital Bone Diseases and Bone Health in Children and Adolescents was established to improve children’s and families' quality of life through treatment, research, and education.
The center, headed by Professor Shlomo Weintroub, a prominent Israeli pediatric Orthopaedics specialist, provides diagnoses, consultations, follow-up, and treatment of children with skeletal dysplasia or other congenital bone diseases—throughout the children’s growth and development. The center’s professional staff works closely with the child and family to provide optimal integrative guidance and treatment.
About skeletal dysplasia
Skeletal dysplasia is a group of about 350 genetic disorders with various degrees of severity characterized by abnormal bone development. It includes different types of short stature and dwarfism. Bone diseases are often accompanied by other disorders, either primary orthopaedic, such as joint dislocation, or secondary, such as fractures. Skeletal dysplasia diseases can impact development and are often accompanied by hearing or sight impairments, hormonal, cardiac or renal problems or digestive tract disorders. At times, the affliction affects neurological, respiratory or psychological functioning.
Although skeletal dysplasia diseases are rare, their overall incidence is approximatively 2.4 per 10,000 births, and about 5% of the genetic disorders in children. Mortality rates range from 0.95 to 1.5 per 10,000 births. In Israel, there are 40-50 new cases annually.
Diagnosis and treatment at the multidisciplinary center
Skeletal dysplasia is diagnosed by clinical and molecular genetics criteria, radiographic imaging and other imaging methods. Today, medicine understands the genetic background of most of these diseases, which facilitates accurate diagnosis. In some cases, the condition can be diagnosed prenatally.
The multidisciplinary center brings together specialists from a variety of fields to provide the most comprehensive care for the child. It functions under the auspices of the Department of Pediatric Orthopaedics at Dana-Dwek Children's Hospital. For more information see the center’s webpage.