Dedicated to the study of basic mechanisms of neuro gastroenterology – the complex interaction between our gastrointestinal (GI) and neurological systems.
Background:
Dysfunction of the intricate neurological system which controls our gut is common in multiple gastro-intestinal disease states, resulting in both motor and sensory symptoms (including abdominal pain, diarrhea and/or constipation). This dysfunction can be secondary to gut inflammation as seen in patients with inflammatory bowel disease. In other disease states, for example irritable bowel syndrome, gut-nerve dysfunction is present but its origins remain unexplained, limiting treatment options. Neurological dysfunction can target different levels of gut innervation, including the intrinsic enteric neuronal network, extrinsic autonomic control, afferent signaling or central processing. Our lab aims to decipher the basic mechanisms for neuronal-gut dysfunction, with a focus on sensory afferent outflow and symptoms. This will ultimately lead to new selective treatment platforms targeting visceral pain with a real aim to enhance the quality of living of our patients.
Lab Team
Research Projects
1) Defining the functional role of pruritogenic receptors in the gut
2) PainBow mapping of colorectal afferents Normal defecation and continence relies on intact colorectal motor and sensory function. The coding of sensory information from the colorectum (pelvic sense of fullness, urge to defecate, pelvic or abdominal pain), depends on the stimuli site (rectum vs. colon). Although site-specific sensory pathways from the colorectum have been described, direct visualizing and detailed characterization of these pathways has proven to be difficult, and overlap and changes in disease conditions are unexplored. In the current project, colorectal afferent pathways to the different spinal cord segments will be mapped, importantly accounting for overlap in innervation in health, colon inflammation and post-inflammation states. To achieve this, we use a unique retrograde tracing technique (PainBow), concurrently injecting multiple dyes in adjacent target organ segments allows us to precisely map overlapping and non-overlapping neuronal projections. Insights gained, coupled with functional testing, will pave the way for understanding and treating site-specific gut symptoms. Highlight Publications
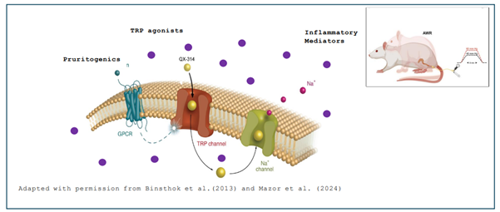
The mechanisms underlying non-painful gut symptoms, such as tenesmus (a false urge to defecate) and defecation urgency, are largely unknown. In my lab we study whether these symptoms involve a family of receptors that mediate non-painful sensation in the skin, namely pruritogenic mass related G protein coupled receptors (Mrgpr) and histamine receptors. Mrgpr and histamine receptors are well established as mediators of itch sensation in the skin. These receptors are co-expressed with TRP channels (e.g., TRPV1, TRPA1) which mediate visceral pain; therefore, they may also be involved in gut sensation and, potentially, mediate non-painful symptoms. To test this possibility, we utilize an activity-based silencing approach based on our previous collaboration with the Binshtok Laboratory. This approach is coupled with behavioral, neurophysiological and advanced imaging techniques to define the role of pruritogenic receptors, as well as suspected downstream TRP receptor activation, in painful and non-painful gut symptoms in the rodent model.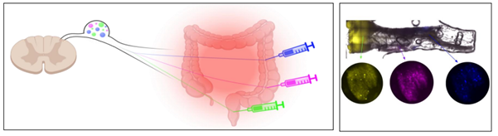
Full list of Research Publications


